Tau: A good protein gone bad
Nearly 6 million Americans are living with Alzheimer's disease, an irreversible neurodegenerative disorder that is currently the sixth leading cause of death in US. The 2020 medical expense for AD is projected to be $305 billion. There is no cure or prevention to date.
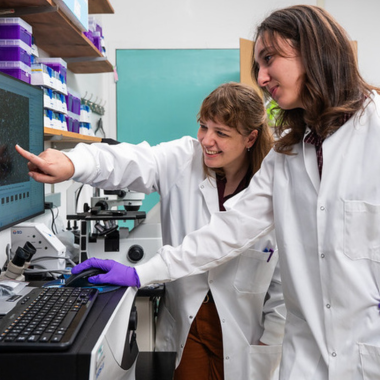
To address this challenge, a team of Michigan State University (MSU) researchers led by MSU biochemist and molecular biologist Min-Hao Kuo, have developed a novel platform to test therapies for Alzheimer’s disease (AD). Much of the work was done by Mengyu Liu, a postdoctoral researcher in the group.
The results of this work were recently published in two journals, Molecular Neurobiology and Scientific Reports.
The progression of cognitive impairments caused by AD, from short-term memory loss, personality change, and the inability to respond to and perform daily activities, is affected by a protein called tau. Tau is predominantly found in the brain and believed to help stabilize microtubules that are essential for the function and structure of axons, the long projection of nerve cells that transmits information to different neurons and muscles.
For some unknown reasons, tau becomes hyperphosphorylated, that is, the phosphate content of this protein increases by several fold in AD patients. Hyperphosphorylation causes tau to lose its original microtubule stabilization activity and triggers tau to aggregate into neurofibrillary tangles (NFTs) in neurons.

“Clinically, NFTs are first found near hippocampus where memory is processed, and eventually spread to the neocortex essential for higher-order cognitive functions, such as spatial reasoning, language, and sensory issues,” said Kuo, who holds a joint appointment in the Colleges of Osteopathic Medicine and Natural Science. “It has become increasingly accepted that the hyperphosphorylated tau plays a key causal role in neurodegeneration in AD.”
For years, research groups have tried to find small-molecule compounds that counter the formation of NFTs, hoping that such compounds would stop or slow down the progression of cognitive decline in AD patients. These studies have not been successful because the subject for drug screening - namely, an “unphosphorlylated” tau, lacked the hyperphosphorylation hallmark for tau in AD brains. It is traditionally difficult to synthesize proteins with the “post-translational modification” (PTM), including phosphorylation. The inability to synthesize hyperphosphorylated tau has impeded the progression of AD drug discovery and disease mechanism studies.
The Kuo group invented a system that enables scientists to synthesize proteins bearing a desired PTM called PIMAX (protein interaction modules-assisted function X). The Kuo team went on to use this system to synthesize hyperphosphorylated tau for the screening for compounds that control NFT formation and prevent neuron death associated with tau pathology. A suite of assays was implemented to find chemicals with the potential to either counteract or to promote AD progression via the changes of p-tau behavior under the influence of each of the test compounds. The former category, that is, inhibitors for p-tau aggregation, contains therapeutics candidates, whereas the latter, p-tau aggregation enhancer category may indicate risk factors for AD.
Of the 1280 compounds that were tested in their pilot screen, two active prescription drugs were found to be of potential therapeutic value for AD. The first one is apomorphine, currently used to control Parkinson’s disease symptoms. An animal study showed that apomorphine preserves the memory of mice engineered to exhibit certain AD symptoms. The second drug, raloxifene whose common name is Evista, by Eli Lilly, treats osteoporosis in postmenopausal women. A clinical trial showed that raloxifene can reduce the chance of cognitive impairment by 33 percent. These two drugs may preserve cognition by counteracting the toxicity of p-tau.
The Kuo group also discovered a subset of benzodiazepine drugs that promote the aggregation and toxicity of p-tau. Benzodiazepines are among the most prescribed drugs in the world. Many seniors, the most vulnerable population to AD, rely on benzodiazepine drugs to battle an array of neurological and psychological conditions.
“Epidemiological studies revealed alarming association between long-term use of benzodiazepines and dementia,” said Kuo. “The discoveries from our team point to a probable explanation for the association between benzodiazepines and cognition. Our methods may provide a means to conveniently differentiate "AD-safe" from "AD-unsafe" benzodiazepine drugs, or any other tentative AD risk factors, leading to the development of effective AD prophylaxis.”
The Kuo group is also collaborating with Cayman Chemical Company in Ann Arbor to develop commercial kits of p-tau aggregation and cytotoxicity for scientists worldwide to do their own tests for AD therapeutics and risk factors. These projects are funded by two grants from the National Institute on Aging, with a combined award of more than 3.1 million dollars.
Banner Image: NFT clinical sample, provided by Dr. Howard Chang, MD, PhD, Department of Neurology MSU, and Sparrow Hospital, and processed by Amy Porter at the Integrative HistoPathology Laboratory, MSU.